Should I Become a Medical Biller or Coder?
This is a great time to consider beginning a career as a Medical Biller or Coder! As the American healthcare system modernizes, there is an increased focus on health data and the digitization of medical records. As a result, there is an increased demand for skilled billing and coding specialists. According to the U.S. Bureau of Labor and Statistics, the medical billing and coding field is expected to grow 13% by 2026, creating nearly 30,000 new jobs in the next seven years. In a field as promising as this one, it’s easy to see why so many students are turning to Asher to learn the skills to become a Medical Biller or Coder!
Medical Coders and Billers work hand in hand to translate healthcare services rendered into requests for payment from insurance companies. First, a Medical Coder codes individual patient services and diagnoses, then a Medical Biller uses those codes to request payment from the patient’s insurance company. Together, these two positions perform a vital administrative task of healthcare, freeing doctors and other medical staff to provide care to patients. In some offices, these two jobs are performed by the same person.
Here is a look at each of these positions in more detail:
Medical Coder-
Medical coding is like translation. Every part of a patient’s medical visit is recorded by a doctor or someone in the healthcare provider’s office. The Medical Coder then translates each bit of relevant information, such as a doctor’s diagnosis, into the corresponding alphanumeric code, which is given to the Biller. For every medical procedure, injury, illness, and diagnosis, there is a corresponding medical code. There are thousands of medical codes, and these codes act as a universal language between doctors, hospitals, and insurance companies.
Medical Coders must be familiar with the codes used in the industry, and also understand the guidelines and rules of the codes. Accuracy and adherence to guidelines is imperative as it can affect the status of an insurance claim. The coding process is complete when the Medical Coder enters the appropriate codes into a form or computer program; once a report is coded, it is passed along to the Medical Biller.
Medical Biller-
The Medical Biller ensures the medical provider is properly compensated for their services by taking the codes produced by the Medical Coder and turning them into a financial report. A Medical Biller takes the information from the Medical Coder and makes a bill for the insurance company, called a claim. The Biller sends the claim to the insurance company. Once the charges have been processed, the medical provider receives paperwork that explains what was paid to the medical provider and what is the patient’s responsibility. The payer also sends an explanation of benefits to the patient, showing what was paid to the provider and their responsibility. The Biller then sends a monthly statement to the patient showing their balance owed the medical provider. If a patient is delinquent or unwilling to pay the bill, the Medical Biller hires a collections agency to ensure the medical provider is properly compensated for their services.
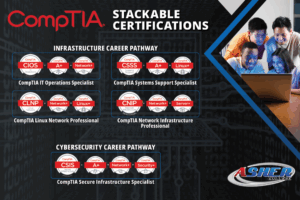
Individuals that graduate from Asher’s Medical Billing and Coding program will be trained in the skills they need to enter this rewarding healthcare field. Asher’s Medical Biller/Coder program can be completed in as few as 40 weeks. Students in the Asher program learn medical coding, billing, filing insurance claims, medical billing software, and medical terminology and anatomy. Asher students will be prepared to test for several certifications, including the Certified Professional Coder-A (CPC-A) and the Certified Professional Biller (CPB), from the AAPC certifying agency or the Certified Medical Administrative Assistant (CMAA), the Certified Electronic Health Record Specialist (CEHRS), or the Certified Billing & Coding Specialist (CBCS) from the National Healthcareer Association. Asher also offers a shorter Medical Records programs as well as a Health Information Specialist program for those seeking to enter the industry and possible have more patient interaction. Asher graduates are trained and ready to immediately begin in entry-level positions in the field. Graduates from Asher’s program can expect to find work as a Medical Biller, Medical Coder, Medical Office Administrator, or Electronic Health Records clerk, and may work in a variety of medical environments including private medical practices, medical billing companies, hospitals, clinics, and insurance companies.
To find out more about Asher College and our Medical Coding and Billing program or Medical Administration programs in Dallas, TX, Las Vegas, NV, or Sacramento, CA, contact us today! Our friendly and helpful Admissions Representatives are always available to you to discuss career options, financial aid and veteran benefit programs, schedule a tour at one of our campuses, or assist you in the enrollment process. Don’t put your future on hold any longer, call Asher at (888) 211-8829 today!